
The voice of the patient is evident in the efforts of the American Joint Replacement Registry (AJRR) largely because of contributions from the Public Advisory Board (PAB). The mission of the PAB is to improve the value of AJRR by even more effectively ensuring a public voice in the Registry's hip and knee replacement data collection, reporting, and utilization activities. Each year, PAB members play an important role in compiling a Report to the Public About Hip and Knee Replacements. The Report's registry-driven, evidence-based content is invaluable in answering the most frequently asked questions (FAQs) from patients and their families. Well-informed patients, with current information, will seek better care and gain better outcomes.
This week's blog focuses on the Report to the Public's answers to patients' FAQs. As a complement to the Report, the blog also features Richard Seiden's account of his personal joint replacement experience and the general patient advice he is sharing through an article he recently authored. He has been a PAB member since 2016.
AJRR 2017 Report to the Public
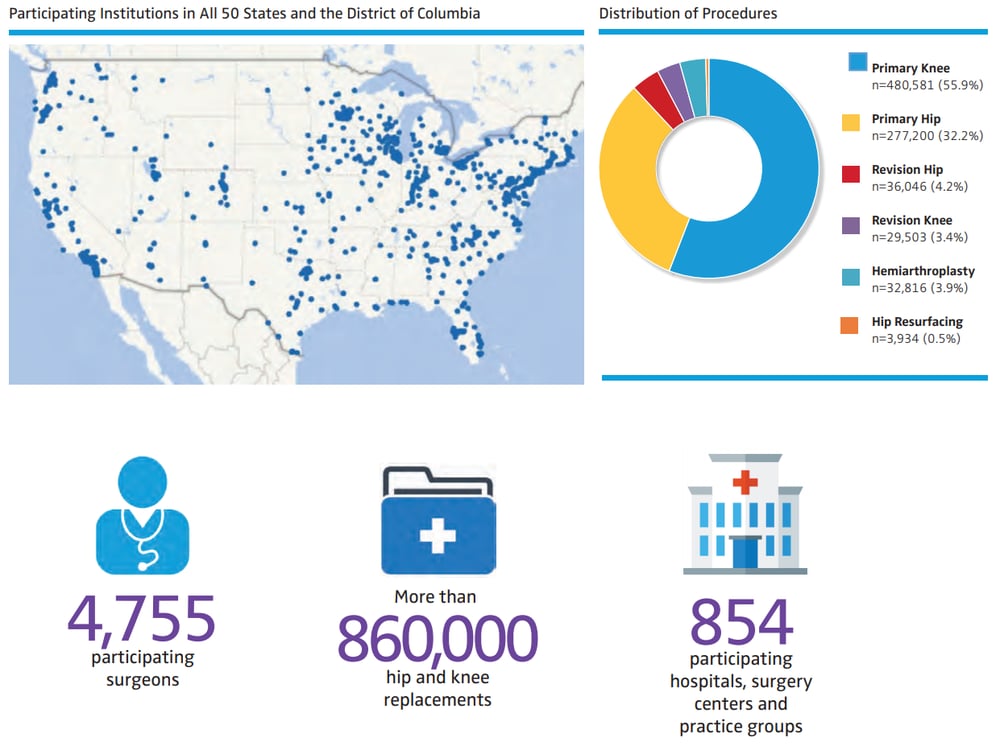
The AJRR mission is to improve care through data for patients who receive hip and knee replacements. Data collected will be used by doctors (for process improvement), surgeons (to evaluate replacement materials), hospitals (to study patient safety practices), medical device companies (to see how products perform), and patients (to understand their treatment plan). Here are some quick facts about the Registry from the latest public report:
FAQs About Hip and Knee Replacements
Q: What kind of information is in the Registry?
A: All joint replacement patient information is privacy protected and includes: age/sex, name of surgeon/hospital, primary (first-time)/revision (re-do) surgery, reason for procedure, recorded complications, and type of artificial joint parts used.
Q: How do I know if my hospital participates in the Registry?
A: You can visit www.ajrr.net to see if your hospital, surgery center, or private practice group is providing data to us. Or you can ask your surgeon.
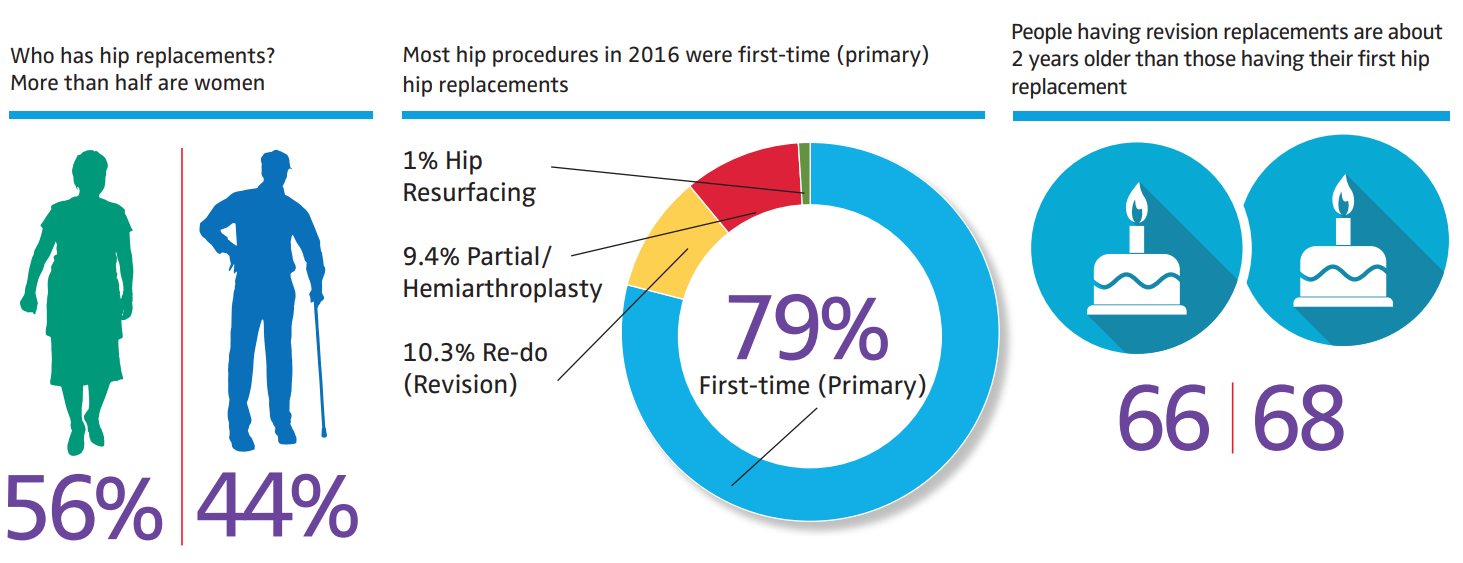
Q: Why do people have hip replacement surgery?
A: Almost 80% of primary hip replacement operations are done to relieve symptoms of osteoarthritis. About 10% of hip replacements are done to treat a hip fracture.
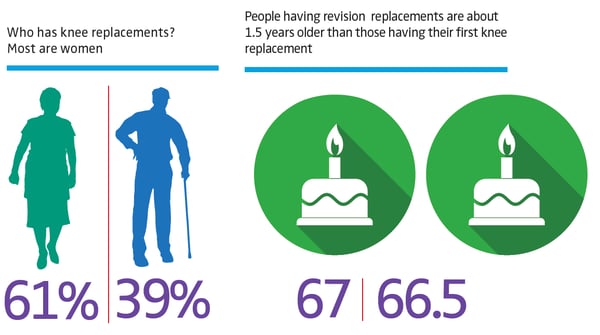
Q: Why do people have knee replacement surgery?
A: About 83% of knee replacements are operations done to relieve symptoms caused by osteoarthritis.
Q: Why is there value in patient-reported outcomes (PROs)?
A: A PRO is information on the results of health care that comes directly from patients without being modified or interpreted by health professionals. It is generally collected through a web-based survey process. When combined with clinical assessment, it provides a 360-degree view of the patient's healing and functional status.
>Listen to a patient describe why he chose to participate in a patient-reported outcomes program.
Q: How do health care institutions select the PRO measures they use?
A: An institution that is utilizing PRO measures to improve clinical care, rather than academic research, will focus on outcomes of physical function and critical symptoms like pain, fatigue, mood, and patient satisfaction. These self-reported domains are measured before and after the procedure to determine if quality of life has improved. By reporting as you progress through recovery, health care providers can make better decisions for patients now and in the future.
A Patient Perspective on Joint Replacement Surgery
Complementary to the AJRR 2017 Report to the Public, PAB member Richard Seiden shares general advice from his personal experience as a joint replacement surgery patient. A Patient Perspective on Joint Replacement Surgery can be reviewed by patients with joint issues to better prepare them for dealing with pre-, day-of-, and post-surgical needs. Mr. Seiden's article content is not a substitute for physician recommendations. Read an excerpt below.
Day of Surgery
An excerpt from A Patient Perspective on Joint Replacement Surgery by Richard Seiden
Since you will be unable to eat anything after midnight on the day before surgery, it is always best to schedule an early time for the surgery itself. This will avoid headaches from lack of food and water, and it usually assures a timely start of the surgery (since there will be no backup from prior surgeries by the same surgeon on your scheduled day). An early start time also lessens anxiety and possible rising blood pressure.
You will probably meet your anesthesiologist for the first time on the day of surgery. Please make sure that they have reviewed not only your primary medical history, but particularly any difficulties you may have had with prior anesthesia experiences. For example, if you have had problems with intubation through the mouth (due to neck issues), please advise the anesthesiologist that intubation should be through the nose.
If your surgery involves your lower extremities (hips or knees), you should discuss with your surgeon and the anesthesiologist the possibility of using a spinal block rather than intubation. A spinal block, combined with a light sedative, can put you in "twilight," or a heavier sleep while in the Operating Room. You can quickly be restored to normal cognitive function (as early as when the surgery is completed in the Operating Room) so you can avoid spending time in Recovery coming out of general anesthesia. This will enable you to be relocated to a hospital inpatient bed sooner than otherwise would occur. The same type of block, called a scalene block, may be used with upper extremity surgery and also limits the amount of general anesthetic that you will need.
Typically, the surgeon will step out into the Waiting Room to advise family and friends of the outcome of the surgery. Otherwise, the surgeon should visit the patient either later the day of surgery or early the next morning. On that visit, the surgeon will check the incision, check mobility of toes, and may even check the range of motion of the replaced joint.
In Recovery, it is not uncommon for a patient to develop dry lips when coming out of general anesthesia. This will have been exacerbated by the fact that you have not had any food or water for over eight hours; most hospitals will provide a patient with lemon swabs or ice chips to enable the patient to avoid the discomfort of chapped lips.
For hips and knees, you will be visited by a physical therapist (PT) either the day of surgery or the next day. Surgeons and hospitals have their own protocol as to the first visit. The first step will be for the patient to sit up (with the assistance of the PT). Assuming there is no lightheadedness after a few seconds, the PT will run a belt around the waist of the patient, position a walker next to the bed and will assist the patient to rise from the bed, with one hand on the bed and one hand on the walker. The PT will have their foot behind one or both wheels of the walker so it does not roll. Once the patient is fully erect, the PT will ask if the patient is comfortable standing. If so, the PT will ask the patient to "march in place". If everything is okay with balance and lightheadedness, the PT will ask the patient to take a few steps in the room (with the PT standing at their side holding onto the belt). Assuming all is well, the PT will accompany the patient on a walk down the hallway, stopping whenever it appears that the patient has done enough, and then they return to the room.
Later in the day, the PT will return and have the patient stand, walk in the hallway, and go to a set of stairs where the PT will confirm that the patient can safely raise their repaired leg to climb and descend at least four steps. All things being equal, and assuming all other signs are okay, the patient will be able to be discharged from the hospital. Most hospitals will wheel the patient to the curbside for pickup in a wheelchair. The patient should have a walker in the trunk of the car. Someone else should drive the patient home.
A Patient Perspective on Joint Replacement Surgery will be available shortly. To post the complete article to your website, please contact us at AJRRinfo@aaos.org.
Find hundreds of articles, videos, and resources to help manage your patients' bone and joint health at OrthoInfo.
For information about the AJRR RegistryInsights™ platform, speak with a Business Development Representative at (847) 292-0530 or Request A Demo today!
Be sure to leave a comment in the form below!


