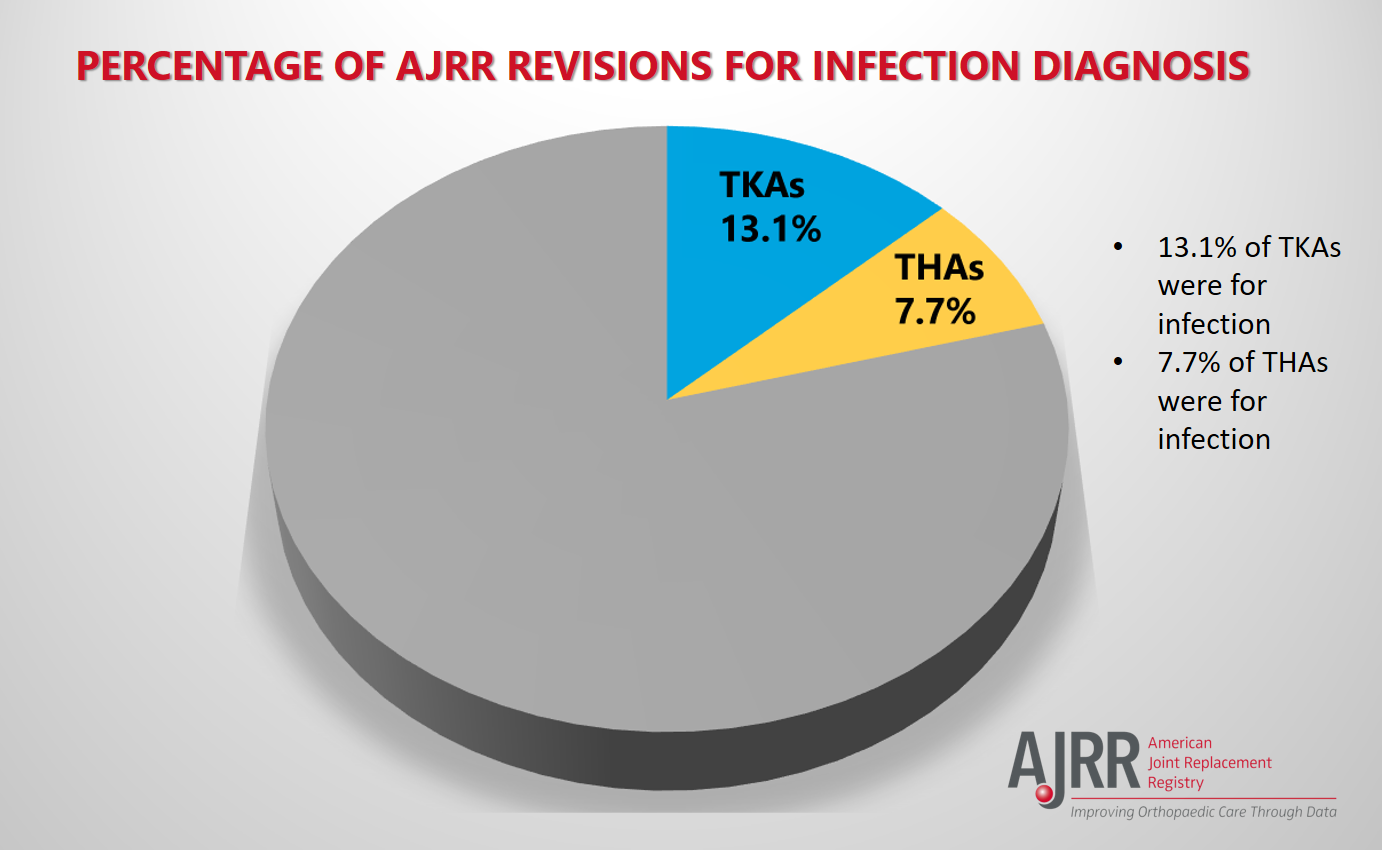
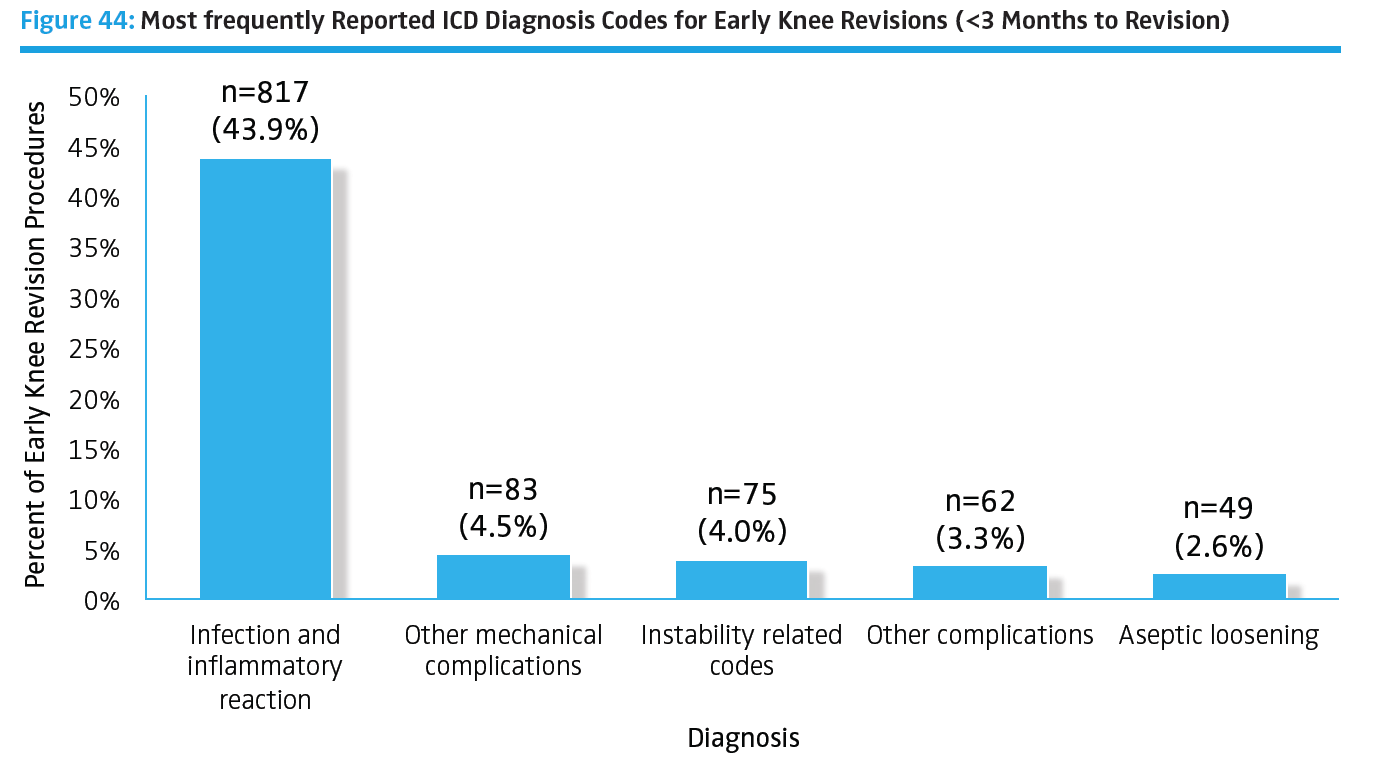
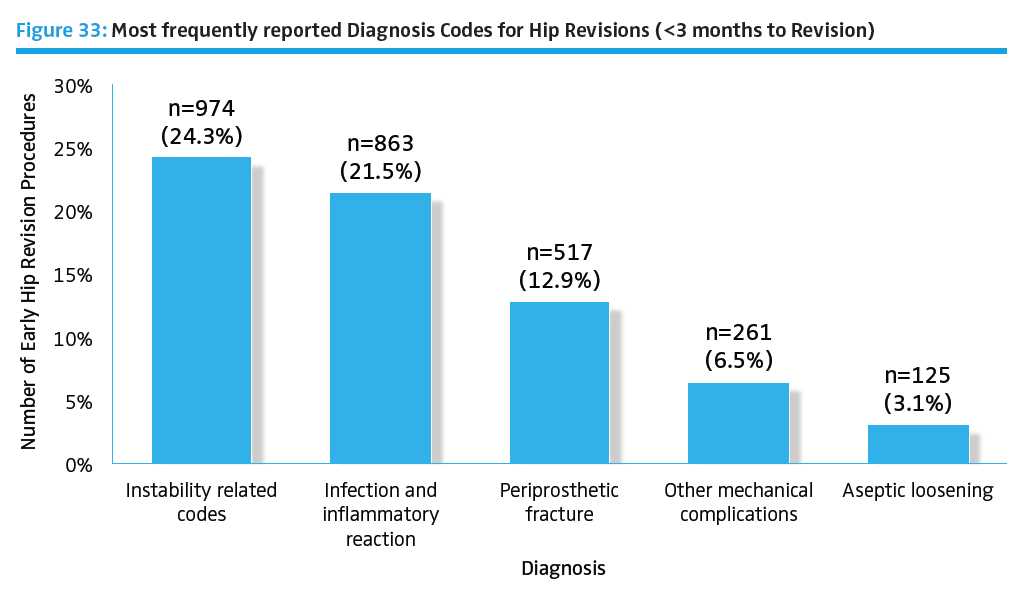
In the American Joint Replacement Registry (AJRR) 2017 Annual Report, infection was identified as a leading cause of total knee arthroplasty (TKA) and total hip arthroplasty (THA) revisions from 2012 to 2016. The majority of early (<3 months) linked TKA revisions are for infection. The majority of early (<3 months) linked THA revisions are for dislocation, infection, and periprosthetic fracture. With an increasing number of TKA and THA procedures being performed in the United States, the rate of failure has also increased. In 2017, AJRR compared and analyzed data for infection-related revision surgeries from six arthroplasty registries including AJRR. The authors presented their poster at the International Society of Arthroplasty Registries (ISAR) 6th International Congress (May 2017). The results showed that for both hip and knee arthroplasty, each registry with six-year data showed an increase in infection burden over the period of the survey.
Other independent research has shown failures due to periprosthetic joint infection (PJI) are expected to increase at an annual rate of between 38,000 cases and 270,000 cases by the year 2030.₁ Orthopaedic registry reporting does not yet capture all institutional data, therefore the actual number of US periprosthetic infections may be higher. Using a nation-wide inpatient sample (NIS) data, Kurtz et al. found the relative incidence ranged between 2.0% and 2.4% of THA and TKA, respectively.₂ The annual cost of infected revisions in US hospitals is estimated to exceed $1.62 billion by 2020.₃
Diagnosis and management of PJI is challenging for surgeons, in part because there is still significant debate as to the standard definition and ideal treatment strategy. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria was recently published in The Journal of Arthroplasty (May 2018, Volume 33, Issue 5) and builds on previous work sponsored by the Musculoskeletal Infection Society (MSIS).
Intraoperative Techniques That Reduce Infections
In a recent issue of Orthopedics Today, AJRR Steering Committee Vice Chair Bryan D. Springer, MD, commented on select trends which have changed some intraoperative techniques used by orthopaedic surgeons to reduce or prevent PJI.₁ 
- Administration of the appropriate dose of antibiotics at the appropriate time during a surgical case has been shown to reduce PJI risk. The standard of care has been to administer three doses of antibiotics - one at the start of surgery and two during the hospital stay. Dr. Springer commented on a new approach: "The CDC has recently come out with guidelines that say you only need one dose of antibiotics and it is creating a lot of controversy because many thought that recommendation is based on either flawed data or data that were not applicable to joint replacement patients." He added, "The best way (to be a good antibiotic steward) is to follow the guidelines that are out there that are evidence-based."
- Use of diluted betadine during surgery or toward the end of surgery to decrease intraoperative contamination is gaining acceptance. "There are several other types of irrigants that are out there, but (the dilute betadine lavage) is probably the one that gets the most attention and has, as of right now, the most data around it," he said.
- Hypothermia may also lead to the development of infection. "I advise surgeons to administer appropriate warming of patients to maintain their body temperature," he said. A variety of warming techniques are described in the article.
- PJI may also be acquired through the hospital environment or by the joint becoming seeded with bacteria. Dr. Springer added, "It is the operating room (OR) traffic that is the biggest risk because we know people shed bacteria, so limiting the number of people that come in and out of the OR is important."
- Performing a quick, efficient procedure will reduce the risk of bacteria entering the incision. The closure technique may be more important in reducing PJI risk than the materials used. "I think the most important thing is that you have consistency in how you close a wound," he said.
Read more about additional intraoperative infection fighting trends and techniques here.
Preoperative Optimization That Reduces Infections
Examples of modifiable patient risk factors that may increase a patient's risk of infection include (but are not limited to) diabetes, obesity, and smoking. "Before we get to the OR, the most important thing is picking the right patients and making sure that any unhealthy patients are made healthy prior to surgery," Dr. Springer concluded. A patient's non-modifiable risk factors cannot be changed, but surgeons must identify and consider them prior to deciding on surgical treatment.
Conclusion
Registries like AJRR continue to track THA and TKA revisions in order to identify possible causes (including infection) and help ensure better patient outcomes. It comes down to understanding the issues and the key role the surgeon and the surgical team play in joint infection prevention. As this blog has demonstrated, orthopaedic surgeons and clinical staff work to minimize the risk of infection through methodical attention to prevention before, during, and after surgery.
₁ “Take Intraoperative Steps to Reduce Joint Infection Risk”, Orthopedics Today, January 2018.
₂-₃ “Periprosthetic Joint Infection: Current Concept”, Indian Journal of Orthopaedics (IJO)
https://www.ncbi.nim.nih.gov/pmc/articles/PMC3601222/
For information about the AJRR RegistryInsights™ platform, speak with a Business Development Representative at (847) 292-0530 or Request A Demo today!
Be sure to leave a comment in the form below!

