The demographics and treatment of femoral neck fracture (FNF) patients have evolved over time. Today's blog uses data from multiple sources to provide orthopaedic surgeons with insights and decision support regarding changing trends in FNF clinical practice. Our primary source is the American Joint Replacement Registry's (AJRR) 2017 presentation at the International Society of Arthroplasty Registries (ISAR) Annual Meeting*. Since the presentation, AJRR has continued to analyze new FNF Registry data and will again share findings at ISAR's 2018 meeting. Our second notable source is a published study in The Journal of Bone and Joint Surgery: "Nationwide Analysis of Femoral Neck Fractures in Elderly Patients" (Volume 99-A, Number 22, November 15, 2017)**.
FNF Treatment History
Arthroplasty for proximal femoral fracture remains a commonly performed procedure with an aging but active demographic in the United States. Options for stem fixation include cemented and cementless designs, with significant variation in usage findings across a variety of databases including registries. Cementless designs are generally reported to have higher rates of intraoperative and perioperative periprosthetic fractures. FNF is a disabling and expensive condition with an estimated U.S. economic burden in the billions of dollars per year. Total hip arthroplasty (THA) for FNF continues to grow as a treatment choice, as evidenced by data trends from all U.S. data sources reported in this blog.
AJRR FNF Patient Population Insights
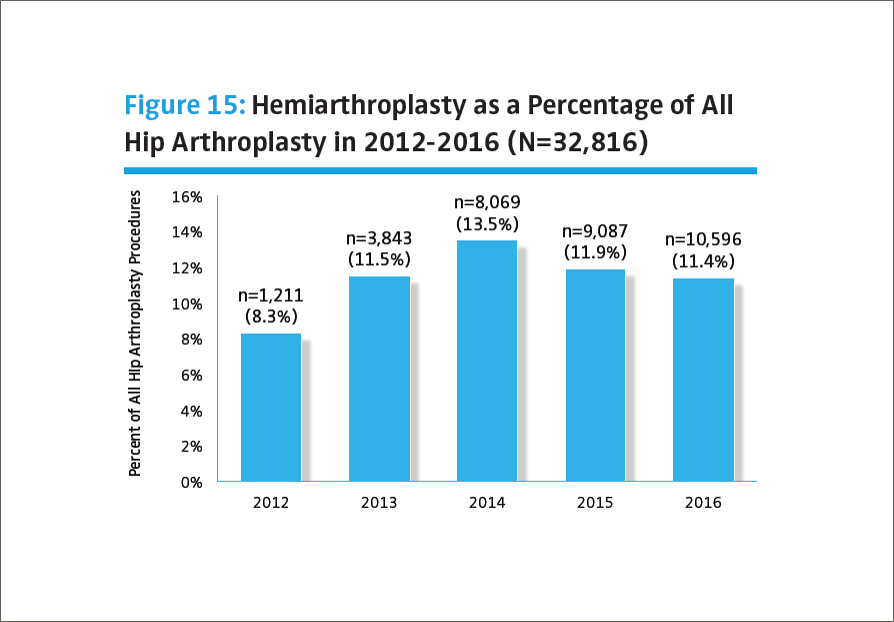
As a national Registry database, AJRR examined arthroplasty treatment of FNF from 2012-2016 regarding: 1) volume trends over time, 2) arthroplasty type: hemiarthroplasty vs. THA, 3) mode of femoral fixation, and 4) surgeon case volume. Throughout a three-year period (ending at the close of 2015), 14,432 hemiarthroplasties were performed for the FNF diagnosis, representing 8% of all Registry arthroplasty procedures. The results of the AJRR analysis of this data are summarized below:
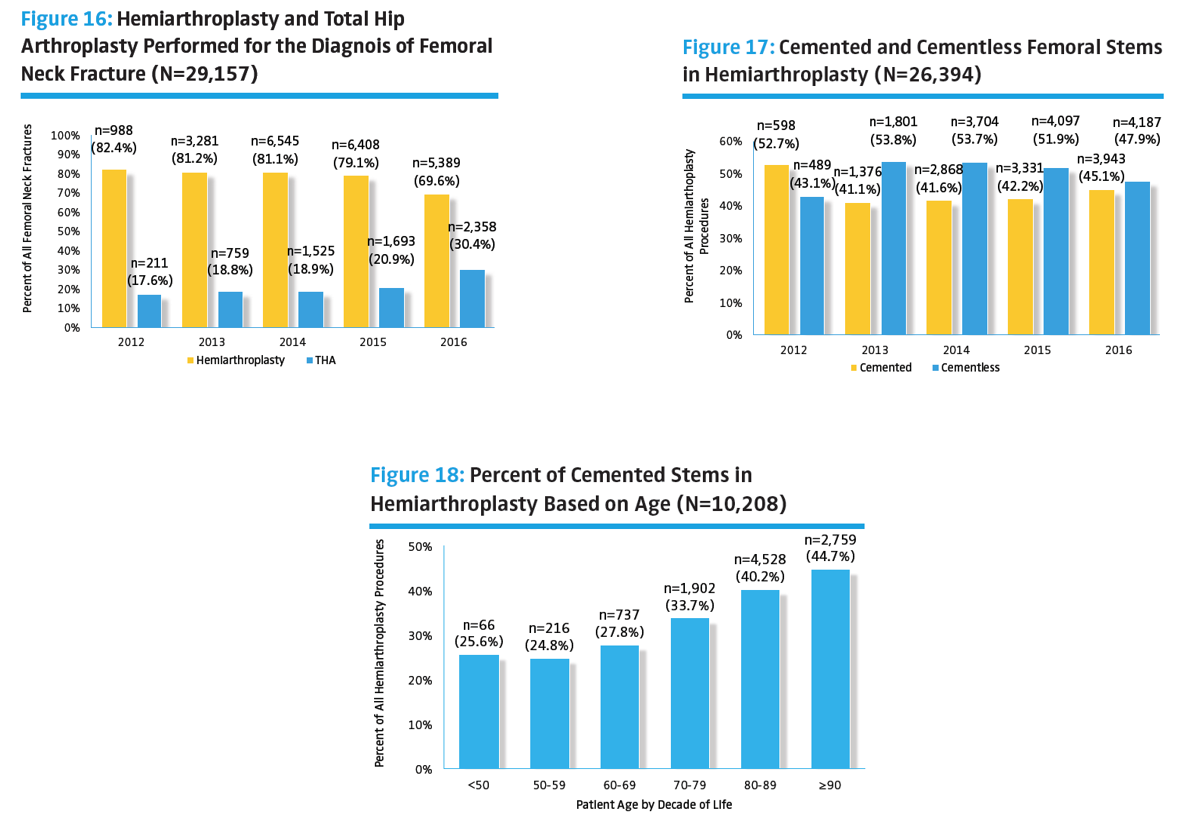
- Since 2013, U.S. surgeons have favored cementless fixation designs in treating FNF.
- In 2012, 38.2% of stems were cementless. Usage increased to 50.3% in 2013 and 54.5% in 2014.
- There is a significant (p<0.001) trend toward greater cemented stem usage with each additional decade of life from 50>90 years of age. However, even in the 80 to 90-year-old age group, <50% of femoral stems are cemented.
- Other national registries generally report much higher cemented stem usage in this setting: 65% in 2015 for the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) and 72% in 2016 for the United Kingdom's National Joint Registry (NJR).
- Of the 22 hemiarthroplasties reported as revised for periprosthetic fracture in the early (<90 days) period, 21 (95.5%) utilized a cementless design.
- THA for FNF continues to grow; the majority of FNF arthroplasties reported to the AJRR utilize cementless stems and bipolar heads in all age groups.
- In the 50 to 90-year-old age group, bipolar heads are used in the majority of cases with hemiarthroplasty stems (>60%). However, there is a significant trend (p>0.001) toward a greater proportion of unipolar heads (compared to bipolar heads) with each additional decade of life.
- The majority (69.1%) of hemiarthroplasties for FNF were performed on females, and the average age of the patients undergoing hemiarthroplasty for proximal femoral fracture is 80 years old.
Journal of Bone and Joint Surgery FNF Older Adult Patient Insights
Only patients ≥65 years old were included in this study to represent the elderly population. As such, the study provides a useful complement to broader AJRR FNF findings shared earlier in this blog. The analysis focused on the most recent 2013 National Inpatient Sample (NIS) data in order to provide an up-to-date analysis of patterns and outcomes in FNF management. Selected results of the analysis are shared below:
- The ten-year study period (2003-2013) shows a steady decrease in the overall incidence of FNF in the ≥65-year-old age group (-25%). The cause of the decrease may be contributing prevention activities like diet, weight-bearing exercise, bone density screening, etc.
- The study identified a modest, but significant longitudinal trend of increasing use of THA in fracture care, with a reciprocal decline in the utilization rate of hemiarthroplasty.
- Hospital costs remained relatively stable, while lengths of stay declined.
- Multiple studies have demonstrated that FNF in older patients have better outcomes when treated with hemiarthroplasty or THA, than when treated with internal fixation.
- THA is associated with the highest initial inpatient hospital costs; however, the long-term benefits from a functional and cost perspective may outweigh the initial disadvantages.
Conclusion
While each of the studies highlighted in this blog have some limitations, they are already providing important indicators for FNF treatment choices. Future data and discovery factors will be better evaluated through prospective, longitudinal studies or registries like AJRR. As the Registry and other national databases grow, additional data about outcomes, revision rates, and indications will undoubtedly influence surgeon FNF treatment choices going forward.
*Gioe TJ, Etkin CD, Cahue SR, Lewallen DG, Berry DJ. (2017, May). Trends in Hemiarthroplasty for Femoral Neck Fracture: Data from the American Joint Replacement Registry (AJRR). Poster presented at the 6th International Congress of Arthroplasty Registries, San Francisco, CA.
**Derek G. Ju, MD₁; Sean S. Rajaee, MD₁; James Mirocha, MS₁; Carol A. Lin, MD₁; Charles N. Moon, MD₁
1 Department of Orthopaedics (D.G.J., S.S.R., C.A.L., C.N.M.) and Biostatistics & Bioinformatics Research Center, Cancer Institute (J.M.), Cedar-Sinai Medical Center, Los Angeles, California
For information about the AJRR RegistryInsights™ platform, speak with a Business Development Representative at (847) 292-0530 or Request A Demo today!
Be sure to leave a comment in the form below!

