AJRR Subscriber Captures the Intersection of Data, Evidence-based Medicine, and Integrated Clinical Pathways
This article was originally published in the July 2018 issue of AAOS Now, the American Academy of Orthopaedic Surgeons' (AAOS) monthly news magazine. It is the second of a three-part series illustrating practical aspects of American Joint Replacement Registry (AJRR) participation through success stories from subscribing institutions. The next installment will feature MountainView Regional Medical Center and appear in the August issue of AAOS Now.
The AJRR is the largest hip and knee arthroplasty registry in the United States, exceeding the 1 million procedures milestone in 2017, and is a part of the Academy’s growing family of orthopaedic registries. TriHealth Good Samaritan Hospital (GSH), located in Cincinnati, OH, has been an AJRR subscriber since January 2015. Other health care institutions can learn from GSH’s registry-supported integrated clinical pathway (ICP) and adverse event (AE) reduction programs focused on blood transfusion, venous thromboembolism (VTE), ineffective pain management, and more.
Prior to participating in the AJRR, GSH had created one of the earliest, most comprehensive, and utilized Level III proprietary registries in the country. The registry is still used in combination with the organization’s AJRR-enabled capabilities to collect Level I, Level II, and Level III data. Figure 1 provides a comprehensive list of all AJRR data elements.
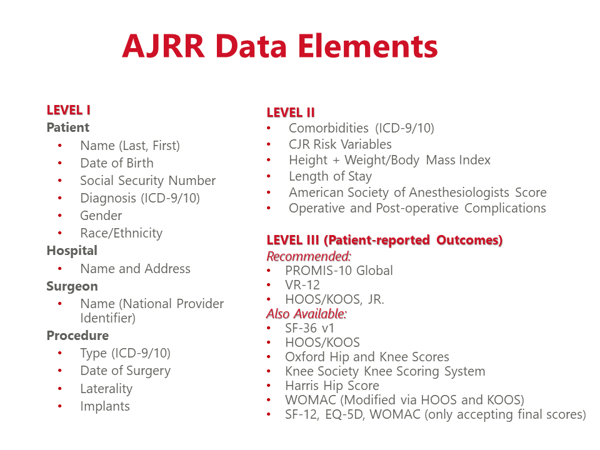
Fig. 1 The AJRR data elements are highly relevant to orthopaedic surgeons, their practices, and the Centers for Medicare & Medicaid Services’ (CMS') reporting requirements.
COURTESY OF AJRR
A six-month transition period enabled GSH to move from its legacy registry to AJRR. The transition required an initial investment, support from surgeon leadership, and an additional full-time employee to manage registry operations.
AJRR’s patient-reported outcomes (PRO) functionality (Level III) includes data required for the CMS Comprehensive Care for Joint Replacement initiative. As a CMS-designated Qualified Clinical Data Registry, AJRR collects 38 measures that are highly relevant to the majority of orthopaedic surgeons, their practices, and their CMS reporting needs.
GSH Launches AE-reducing Zero In On Zero Program
Mark A. Snyder, MD, said, “GSH has deployed a novel, AE-reducing Zero In On Zero (ZIOZ) program for total knee and hip arthroplasty patients, which is coupled with Level III registry and facilitates problem solving with evidence-based information.”
All 10 ZIOZ AE initiatives mentioned in this article led to decreased complications, including the following three examples:
- GSH created and integrated an anemia clinic to measure and address complete blood count. The clinic provides treatment of anemia and reduced blood transfusions and related complications to zero over a 12-month period (Figs. 2 and 3).
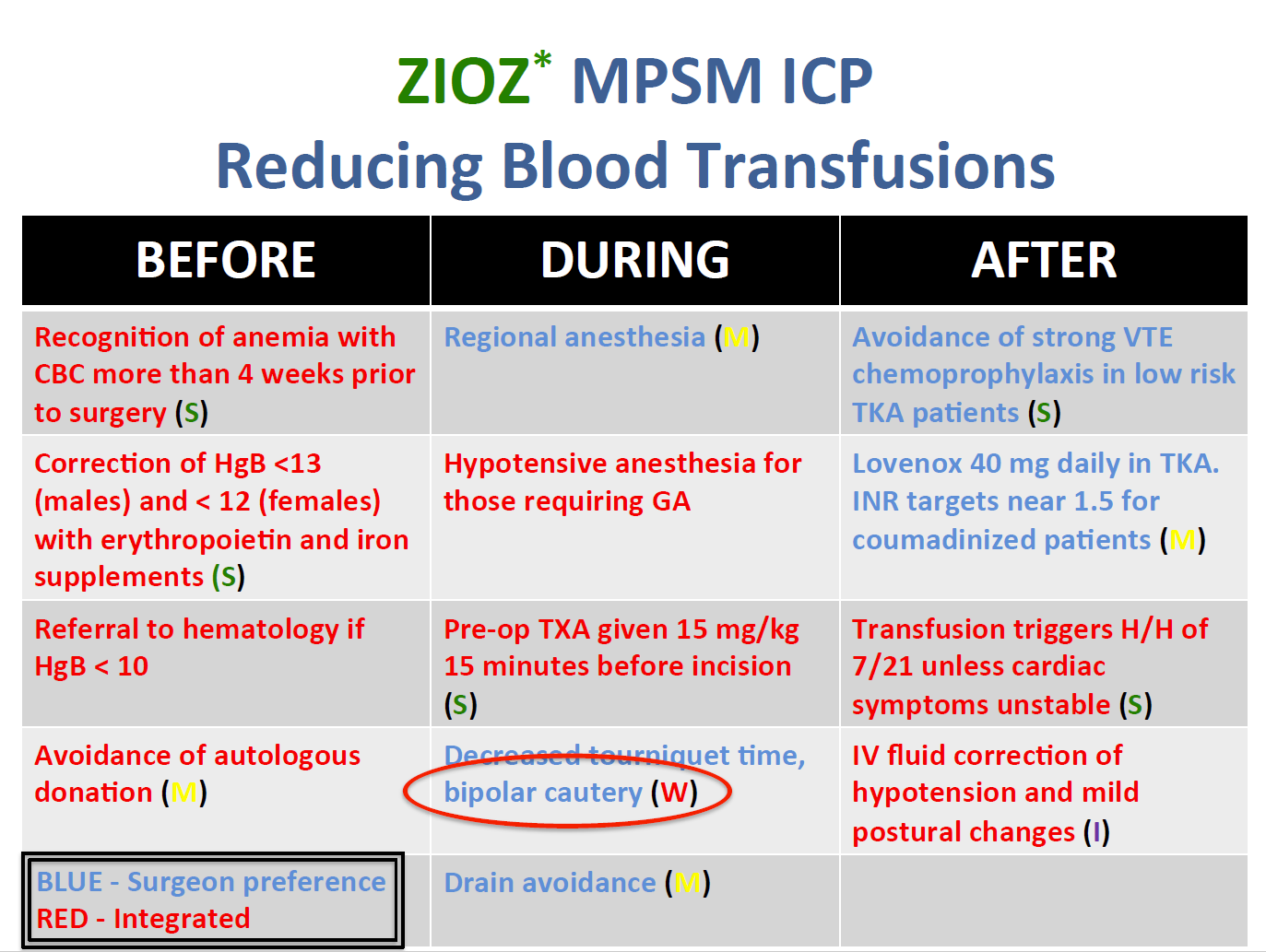
Fig. 2 Within the ZIOZ program for transfusion reduction, the best practice model is structured around three phases of care: before, during, and after the procedure. The best practices in each phase are rated for their effect on transfusion reduction: (S) strong influence, (M) moderate influence, and (I) inconclusive influence.
COURTESY OF TRIHEALTH GSH AND MARK A. SNYDER, MD
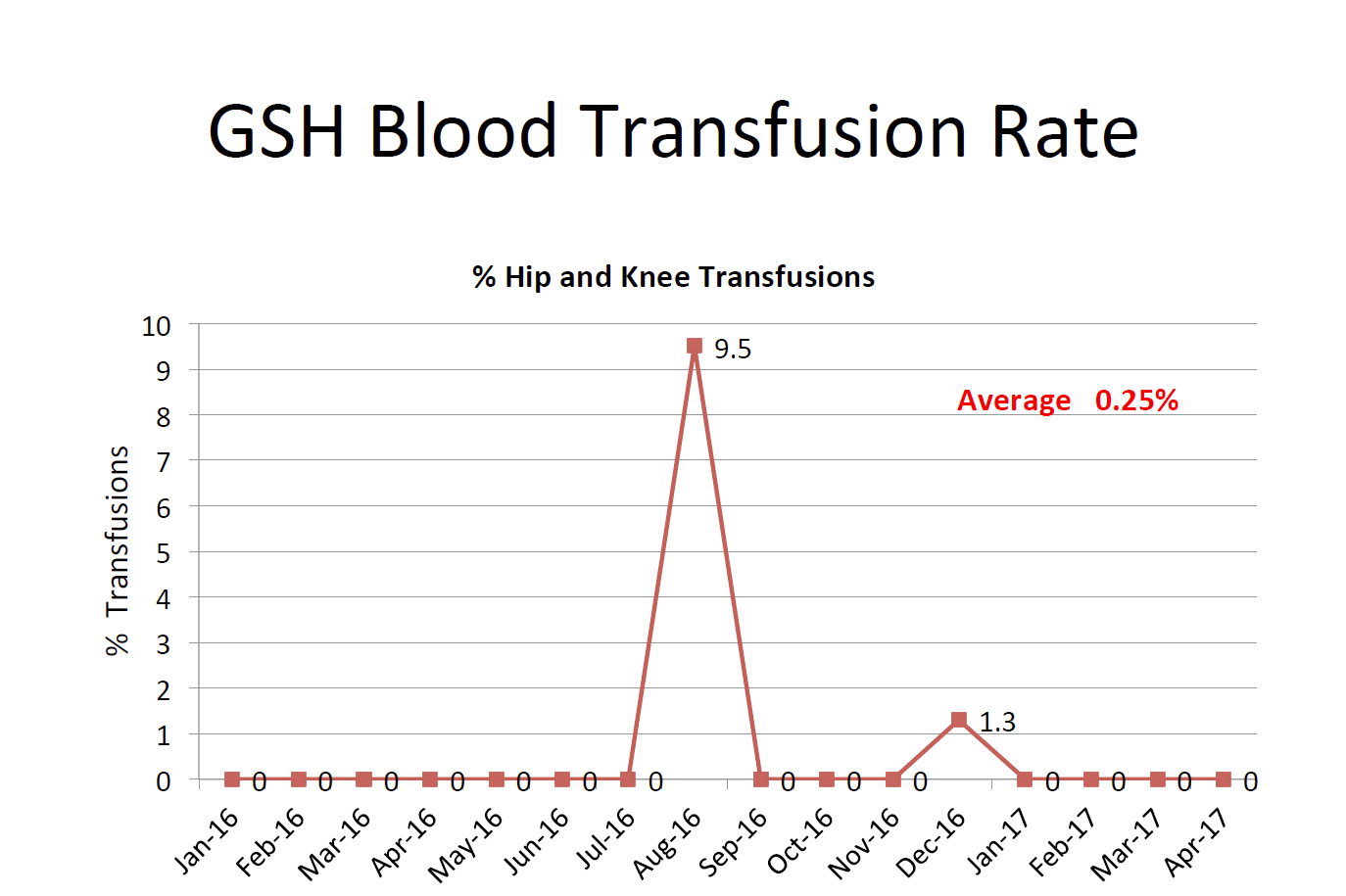
Fig. 3 After experiencing a record high transfusion rate (9.5 percent of hip and knee procedures) in 2016, TriHealth Good Samaritan Hospital reduced and maintained a 0 percent transfusion rate in 2017.
COURTESY OF TRIHEALTH GSH AND MARK A. SNYDER, MD
- GSH purchased mobile compression devices for all total joint replacement (TJR) cases within the system to prevent deep vein thrombosis and VTE, eliminating VTE re-admissions and deaths (Fig. 4).
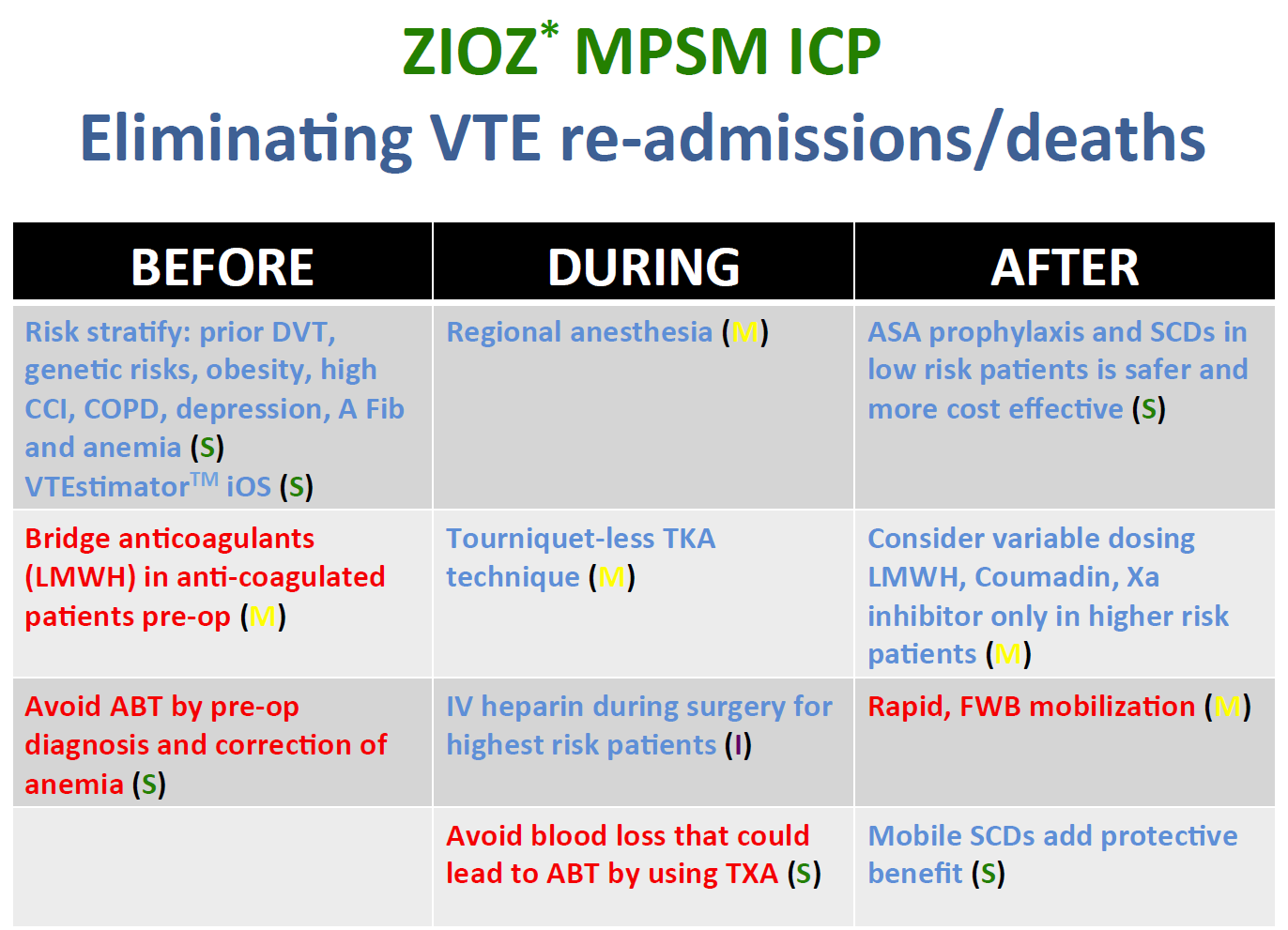
Fig. 4 The ZIOZ program for VTE re-admission/death elimination achieved zero level adverse event outcomes. The best practice model is structured around three phases of care: before, during, and after the procedure. The best practices in each phase are rated for their effect on VTE re-admission/death elimination: (S) strong influence, (M) moderate influence, and (I) inconclusive influence.
COURTESY OF TRIHEALTH GSH AND MARK A. SNYDER, MD
- GSH purchased liposomal bupivacaine for multimodal problem-solving method (MMPM) care to support an opioid-sparing program, thereby reducing complications from opioid use and preventing poor pain management (Fig. 5).
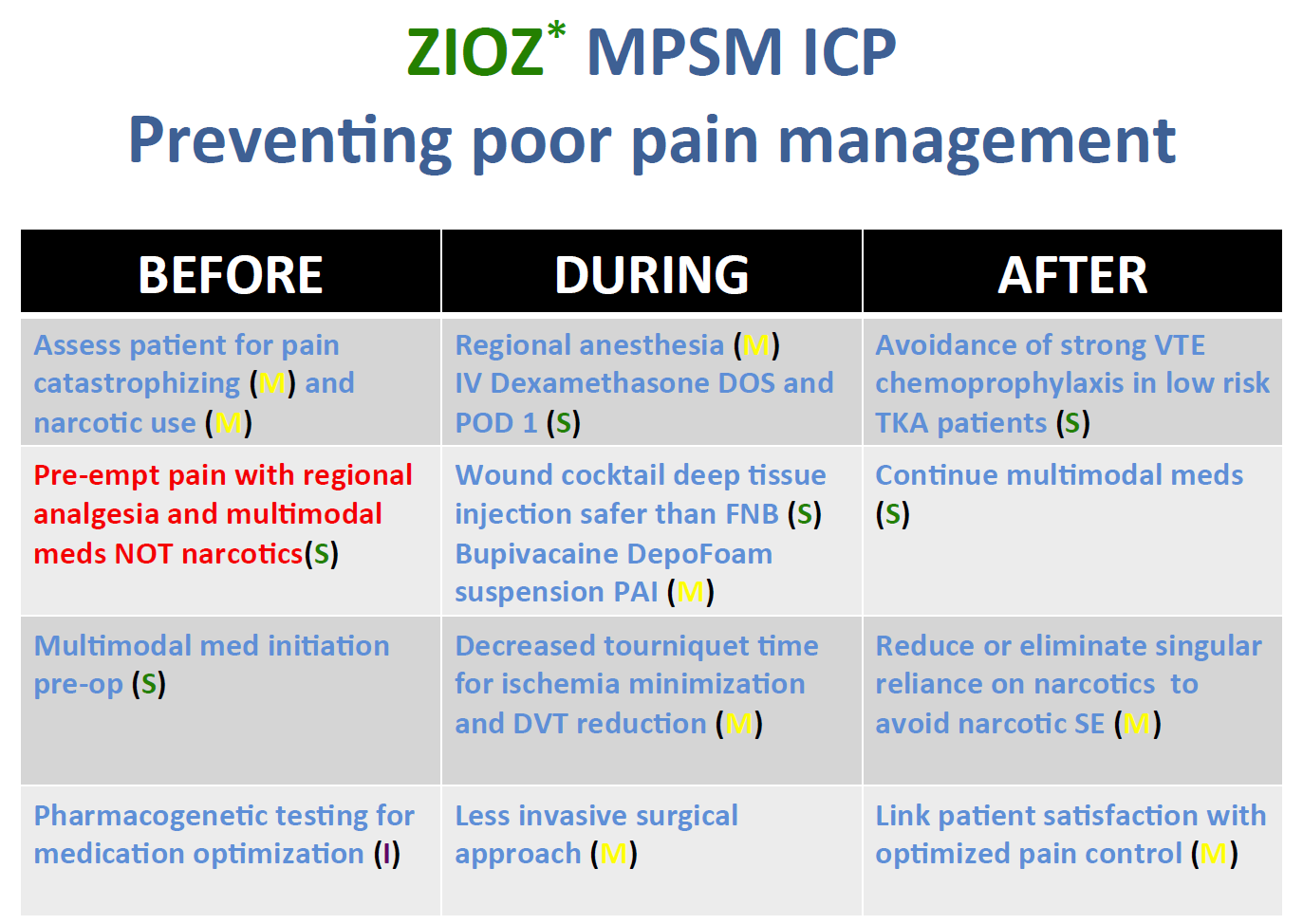
Fig. 5 The ZIOZ program for preventing poor pain management achieved near-zero level adverse event outcomes. The best practices in each of its three phases are rated for their effect on positive pain management outcomes: (S) strong influence, (M) moderate influence, and (I) inconclusive influence.
COURTESY OF TRIHEALTH GSH AND MARK A. SNYDER, MD
Level III registry data formed the background proof of concept for all three efforts.
Defining ZIOZ Practice Concepts
The ZIOZ program combines registry data and supporting practice concepts that empower the analysis of preventable problems and yield meaningful results related to TJR. Components include the following:
- EBM: evidence-based medicine is an approach to medical practice intended to optimize decision making by emphasizing the use of evidence from well-designed, related research
- ICP: integrated clinical pathways are multidisciplinary care plans that detail essential steps in the care of patients with a specific clinical problem
- MMPM: multimodal problem-solving method is relating to, having, or utilizing more than one problem-solving approach
Sharing Meaningful Results
GSH has enjoyed broad Level III registry adoption, which is combined with extensive multimodal problem-solving ICPs. Together, the Orthopaedic Center of Excellence’s TJR efforts have reduced complications, eliminated 30- and 90-day re-admissions by 90 percent, and lowered total episode 120-day costs by nearly 25 percent. Full utilization of the Institutional Review Board-approved Level III registry validated extensive MMPMs for 10 AEs and the rate of 90-day all-cause re-admissions in more than 2,000 primary total hip and knee arthroplasty patients over six years (less than 1.5 percent). The observed AEs, including the three already detailed, are transfusions, infected total hip and knee arthroplasties, prolonged lengths of stay, postoperative urinary retention/postoperative nausea and vomiting, delayed physical therapy, poor discharge handoffs, dissatisfaction, dislocations, patient falls, 30-day re-admissions, VTE-related re-admissions, and ineffective pain management.
Not only does the intersection of Level III registry, EBM, and ICP compliance enable clinical analysis, it also drives collegial consultation between compliant and non-compliant multidisciplinary physicians and surgeons.
“When greater numbers of the medical staff closely adhere to the safety and quality recommendations that come out of this multimodal ICP program, they are more likely to provide optimized PROs and the safest, most cost-effective care,” Dr. Snyder said.
Conclusion
Dr. Snyder stated, “The ZIOZ program is delivering measurable and targeted results at GSH every day. Registry participation tells patients, payers, providers, and points of service that we are serious about eradicating preventable complications, re-admissions, and excessive costs. Our Joint Commission Advanced Orthopaedic Certification is, in part, dependent on registry participation. Without AJRR, we would not have the proof we need for the ICP initiatives, nor the health system push to support initiatives like mobile compression devices purchased for every TJR case. We view [this] program and Registry participation as cornerstones of our current and future quality care delivery efforts.”
Read more in AAOS Now (July 2018 issue).
Karen Metropulos, MBA, is a content writer and blog editor at the AJRR, part of AAOS’ Registry Program.
For information about the AJRR RegistryInsights™ platform, speak with a Business Development Representative at (847) 292-0530 or Request A Demo today!
Be sure to leave a comment in the form below!

