![]()
The information below was featured in two articles published in the June 2020 issue of AAOS Now, the American Academy of Orthopaedic Surgeons (AAOS) monthly news magazine.
The AAOS Registry Analytics Institute® gives clinicians and clinician scientists the opportunity to submit hypotheses about information in AAOS registries. Those with approved proposals receive AAOS analytics insights and committee guidance. Read on for a summary of two recent projects using analyses from the American Joint Replacement Registry (AJRR), AAOS' hip and knee arthroplasty registry.
Dual Mobility Utilization Trends in The United States: An Analysis of the AJRR
A study analyzing data from the AJRR and describing utilization trends of dual mobility (DM) articulations in the United States for primary and revision total hip arthroplasty (THA) found that DM utilization increased year over year during the study period across all age groups. In the final year of analysis, approximately 30 percent of revision THAs and 12 percent of primary THAs used a DM implant. Nathanael Heckmann, MD, FAAOS, of the Keck School of Medicine of the University Southern California, presented the data as part of the AAOS Annual Meeting Virtual Experience.
The study group consisted of all patients with data submitted to AJRR who underwent a primary or revision THA between 2012 and 2018 and had bearing surface data. AJRR has been collecting component information since its inception. As reported in the AJRR 2019 Annual Report, completeness of selected attributes ranges from 57 percent to 99 percent. Patients without implant information were excluded. Patient characteristics, including age and sex, were recorded for each patient. Hospital size and academic affiliation were classified as major teaching institution, minor teaching institution, or nonteaching institution.
Utilization Factors
A total of 406,900 primary THAs were identified in the study period, of which 35,455 (8.7 percent) involved a DM articulation. Among primary THA procedures, DM utilization increased from 6.7 percent in 2012 to 12.0 percent in 2018 (Fig. 1).
Fig. 1: Dual mobility utilization from 2013 through 2018, which showed a year-over-year increase for primary and revision total hip arthroplasty during the period examined
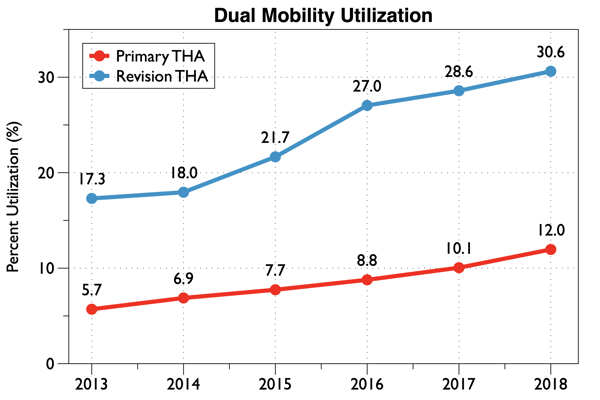
Courtesy of Nathanael Heckmann, MD, FAAOS
During the same time interval, 34,745 revision THAs were identified, of which 8,031 (23.1 percent) involved a DM implant. Among revision THAs, DM utilization increased at an even more rapid rate, with 19.5 percent of revisions involving a DM implant in 2012 and 30.6 percent involving a DM implant in 2018.
When assessing DM utilization by age, the researchers found an increase in usage across all age groups during the study period (Fig. 2).
Fig. 2: Dual mobility utilization by age group from 2013 through 2018; in every year assessed, patients younger than 50 years showed the highest rate of dual mobility utilization. (Note: Data from 2012 were not graphed due to the low number of cases and contributing institutions.)
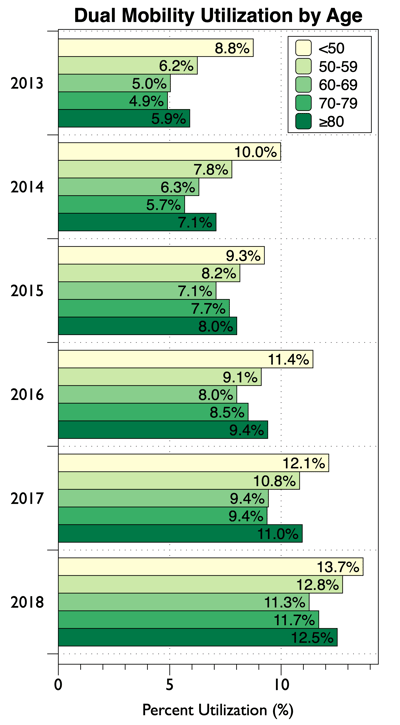
Courtesy of Nathanael Heckmann, MD, FAAOS
Patients younger than 50 years showed the highest rates of DM utilization, increasing from 8.8 percent of primary THAs in 2013 to 13.7 percent in 2018. Patients 80 years or older received DM implants at the second highest rate, increasing from 5.9 percent of cases in 2013 to 12.5 percent in 2018.
The year the surgery was performed was associated with utilization of DM articulations such that for every subsequent year assessed there was an approximately 20 percent increase in utilization of DM implants for patients undergoing primary THA. For every year increase in age, there was a 0.4 percent decrease in the rate of DM utilization. Women were more likely to receive a DM implant than men. Patients undergoing revision surgery also saw a year-over-year increase in utilization of approximately 17 percent.
Patients undergoing primary THA for dysplasia, post-traumatic arthritis, femoral neck fracture, or osteonecrosis were more likely to receive a DM articulation compared to patients undergoing THA for osteoarthritis. Patients undergoing revision THA for instability periprosthetic fracture (PPF), aseptic loosening, or infection were more likely to receive a DM implant compared to patients undergoing revision THA for wear or osteolysis.
Dr. Heckmann said that an unexpected and even “alarming” finding is that DM implants are being used most frequently in patients younger than 50 years, accounting for approximately 14 percent of primary THAs in that age group in the final year of analysis. “This is of particular concern, as the long-term performance of these implants has not been well described,” he said.
A main takeaway of the study, he said, is that further research regarding the implants is required. In particular, Dr. Heckmann said, “More research is needed to identify which patients stand to benefit the most from these implants. More importantly, further research is required to better understand the long-term implications of the trends identified in the current study.”
Value of Registry
Dr. Heckmann said the study illustrates the importance of AJRR as a surveillance tool that can help identify potentially problematic practice trends—in this case, an increasing number of DM implants used in patients younger than 50 years. “This practice could not have been identified or studied using other databases such as the National Inpatient Sample because these databases rely on International Classification of Diseases, 9th and 10th edition, codes to identify bearing couples, and there are currently no codes that identify these types of implants. As such, DM practice trends can only be studied using a database such as AJRR.”
He noted that as with all database studies, the retrospective nature is the biggest limitation. “We are unable to account for specific patient and surgeon factors that lead to DM utilization on an individual level,” he said. “As such, we are unable to account for potential confounding factors. Nevertheless, the limitations do not change the major findings of this study—namely, that DM utilization is increasing, and this increase is happening most in the youngest patients.”
Dr. Heckmann’s coauthors of “Dual Mobility Utilization Trends in The United States: An Analysis of the AJRR” are Dena Weitzman, OD; Heena Jaffri, MPH; Daniel Berry, MD, FAAOS; Bryan Springer, MD, FAAOS; and Jay R. Lieberman, MD, FAAOS.
Migration Patterns Reported in the AJRR for Revision Total Hip Arthroplasty
A study based on data from the AJRR, presented as part of the AAOS Annual Meeting Virtual Experience by Richard Illgen, MD, FAAOS, of the University of Wisconsin, found significant differences in migration rate and destination in patients treated for PPF after THA, with the highest percentage of patients migrating from small nonacademic centers to large or medium academic centers. A similar pattern was noted for revision THA for other causes, but it did not reach statistical significance.
The investigators reviewed AJRR and linked Centers for Medicare & Medicaid Services (CMS) data to evaluate migration rates and destinations based on hospital size (large, medium, or small) and teaching affiliation (teaching or nonteaching) for all revision THAs (n = 25,980) and revision THAs for PPF (n = 892). All primary and revision THAs for patients 65 years or older as reported to AJRR from Jan. 3, 2012, to Sept. 26, 2018, were included. Cases were linked with CMS data for cases from 2012 to 2017.
Cementless stems were 2.6 times more likely to undergo early revision for PPF than cemented fixations. The overall migration rate was 0.32, and no significant difference was seen by hospital size or teaching affiliation. Migration destination for revision THA differed by hospital size; 19.1 percent migrated to small hospitals, 36.8 percent to medium, and 40.3 percent to large. Regarding teaching affiliation, 66.7 percent of cases migrated to a teaching institution. Migration rates for PPF revisions showed statistical significance comparing small hospitals (0.36) to medium (0.17, P < 0.001) and nonteaching (0.31) to teaching institutions (0.23, P < 0.01). PPF was the most common cause for early revision THA (less than three months), with a similar rate in all groups (15.6 percent to 18.3 percent).
Overall, the results showed that patterns of migration differed for revision THA based on hospital size and teaching affiliation. Large hospitals and teaching institutions are the preferred destinations for revision THA (Table 1), with demonstrated statistical significance when revision THA for PPF was analyzed (Table 2). PPF was also the most common cause for early revision THA for all hospital sizes and teaching affiliations.
Table 1: Overall migration rates and migration destinations by hospital size and teaching type for patients ≥ 65 years (n = 6,510)
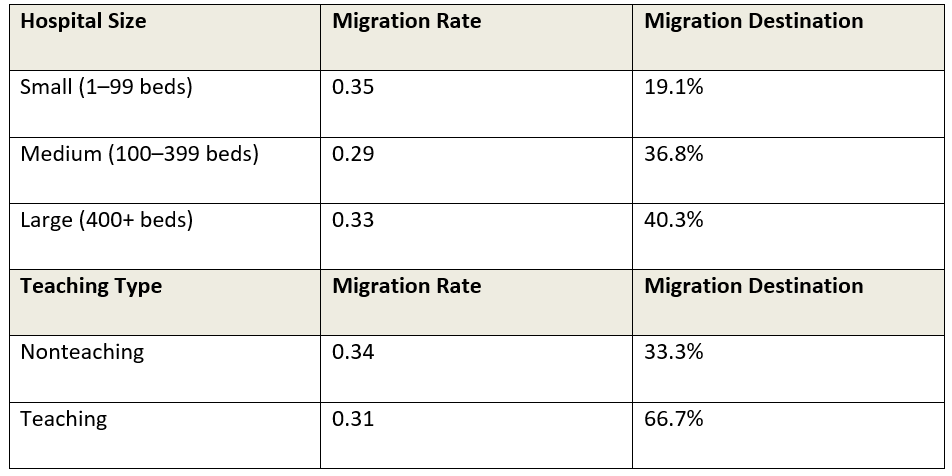
Courtesy of Richard Illgen, MD, FAAOS
Table 2: Migration rates for revision total hip arthroplasty due to periprosthetic fracture (n = 892)
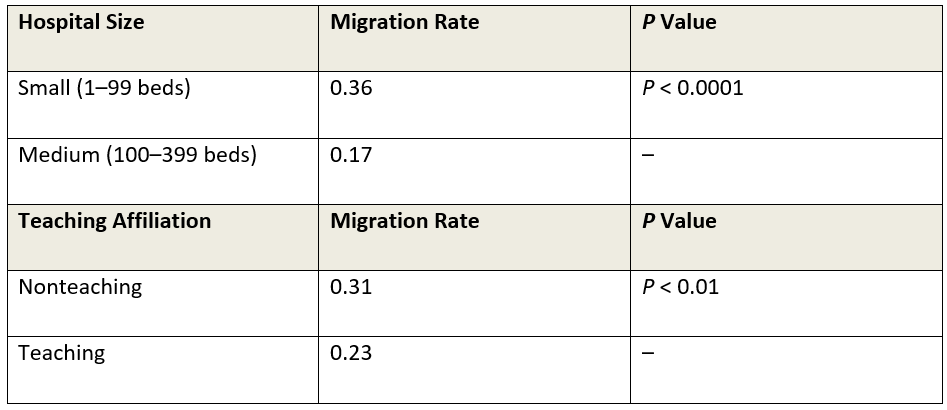
Courtesy of Richard Illgen, MD, FAAOS
Asked whether any findings were unexpected or surprising, Dr. Illgen said, “Rates of migration after THA complicated by PPF were significant, relatively large, and place a significant burden on affected institutions.”
The authors noted that revision THA represents a significant financial burden for the health care system, with the highest costs and complication rates associated with revision THA for PPF. “At present,” they wrote, “the increased cost associated with caring for patients with PPF are not reimbursed adequately by CMS.” They said the volume of primary THAs in the United States continues to rise on an annual basis, with approximately 500,000 procedures per year; it is estimated that the volume of revision THAs will also rise proportionately. Data from 2016 estimated the number of revision THA cases to be between 50,000 and 60,000 cases for that year.
“With national and international registries citing 10 percent to 15 percent of revision THAs being due to PPF, the additional costs associated with treatment can become burdensome for institutions absorbing these cases,” the authors wrote. Previous studies, they noted, have associated cementless femoral fixation with 2.6 times higher risk of early PPF (within 90 days) compared with cemented femoral fixation. “The appropriate use of cemented femoral fixation in at-risk patients for PPF after primary THA could potentially reduce the financial burden, morbidity, and mortality of these complex and challenging postoperative complications,” they wrote.
AJRR: Unique Data Source
Dr. Illgen said he and his colleagues undertook the study because little information had been available regarding migration rates and destinations in THA patients. “The AJRR represents a unique data source to better understand these patterns based on hospital size and teaching affiliation,” he said. “The AJRR provides a unique dataset at the national level, especially when linked to the CMS database, to allow this type of study to be performed. The establishment of the Analytics Institute within the AJRR in February 2019 serves to open the AJRR database to U.S. physician researchers and establishes a straightforward mechanism to utilize this dataset to answer clinically relevant and important questions.”
Dr. Illgen said that further studies are needed to explore other issues related to migration after THA, including state-to-state migration and migration after revision THA. “These follow-up studies are currently being completed utilizing the AJRR and a team of researchers from across the United States,” he said.
Dr. Illgen’s coauthors of “Migration patterns reported in the AJRR for Revision Total Hip Arthroplasty” are David G. Lewallen, MD, FAAOS; Heena Jaffri; Dena S. Weitzman, OD; and Kevin Bozic, MD, FAAOS, MBA.
Apply for AAOS Registry Analyses
If you are interested in utilizing AAOS Registry Program analyses for your next project, you can learn about the AAOS Registry Analytics Institute application process here. The Institute accepts proposals in cycles throughout the year, and cycle 2 is open from June 8, 2020 through July 13, 2020.
Terry Stanton is the senior science writer for AAOS Now. He can be reached at tstanton@aaos.org.
Be sure to leave a comment in the form below!



