Three fundamental goals should stand out when starting a patient-reported outcomes (PRO) program. First, you are determined to evaluate care by including outcomes based on the patient’s viewpoint along with other clinical measures. Longitudinally tracking patient assessment of pain and function can provide insights into the effectiveness of hip and knee arthroplasty across a much broader patient population than the relatively small number of patients that suffer implant failures and require surgery.
Second, you are determined to enable your institution’s provision of PRO data to the Centers for Medicare & Medicaid Services (CMS) and other payers as they continue defining quality measures for value-based reimbursement. For example, CMS defines PRO requirements within their Medicare reimbursement programs such as Comprehensive Care for Joint Replacement (CJR) model and the Merit-based Incentive Payment System (MIPS). MIPS recently replaced the Physician Quality Reporting System (PQRS). The demand for PRO data by regulators, payers, accreditors, and professional organizations has accelerated, as patient care associated with PRO programs has demonstrated improvement. Better technology for data capture has also accelerated demand.
Finally, you are determined to use comparative data and PRO benchmarking to provide evidence for needed quality improvement work at both the hospital and surgeon level. National Registry data is often used to enable this effort.
If these goals are important to your institution, the five steps shared below will help you launch a successful PRO program:
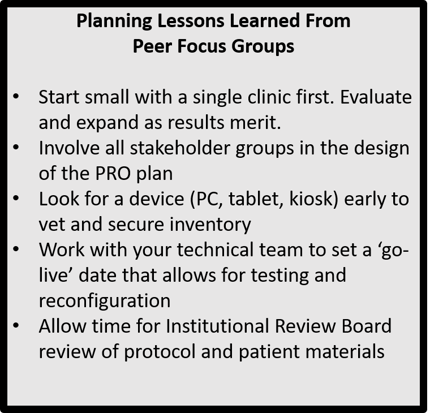
Step #1 – Identify Your Institution’s Key Contributing Stakeholders to PRO Program Development
Launching a PRO program will require a multidisciplinary group within your institution to drive and implement the program. Below is a list of potential key stakeholders who may assist in developing and capturing PROMs for your institution:
- Physician Leadership
- Orthopaedic Department
- Related Practice Groups and Clinics
- Quality Department
- Information Technology
- Orthopaedic Service Line
- Research
- Rehabilitation
- Hospital Administration
- Patient Advocate(s)
Step #2 – Define Your PRO Program Goals
The goals driving implementation of your PRO program, beyond the fundamental three discussed above, can differ by institution. Community hospitals and academic medical centers, for example, have some different needs to address. Key questions that can guide your goal setting choices include:
- Are we launching research initiatives?
- Are we seeking comparative benchmarks nationally, locally?
- Are we quantifying our outcomes from the patients’ perspective?
- Do we want to measure overall health improvement?
- Will patient provided data be used in the clinical encounter?
- Will PROs be used to evaluate quality initiatives?
- What are the requirements of the payer-specific program(s) for which we hope to qualify?
Step #3 – Determine the Appropriate PRO Measure(s) and Timeline
Your reasons for implementing a PRO program will direct your team to the use of certain instruments that will meet the needs of the program’s goals. For example: if you are collecting PROMs for research initiatives, you may choose longer instruments like the HOOS and KOOS, which provide multiple subscales on pain, function, symptoms, etc., that will give a depth of data to address many research hypotheses. If you are focused on measuring patient outcomes as part of clinical care or your research is focused on a specific defined domain (e.g., pain or function), shorter instruments like the HOOS, JR. and KOOS, JR. will work. How often you need to measure change becomes your timeline for data collection. The International Consortium for Health Outcome Measurement (ICHOM) recommends a pre-op baseline and then a one year follow-up for data collection. CMS’ CJR Final Rule defines frequency of data collection similarly.
Step #4 – Develop Workflow for Data Capture
Once you have determined the purpose of PRO data collection, which measures to collect, and your timeline for data capture, you can develop the protocol for data collection. An important and early decision will be choosing a PRO collection tool capable of tracking complete data, presenting PROs in the context of an individual surgeon, surgical approach, implant, etc. This attention to context greatly improves the utility of your data and the ability to interpret it. You can refer to A Buyer’s Guide to Orthopedic Patient-Reported Outcome Collection Tools for help in determining which type of PRO collection tool best meets your needs. For example, does the tool adequately address reporting compliance, data validity, quality improvement, and patient safety considerations. Who owns the completed data after it is submitted by the patient? Are reports produced by you or a vendor? The diagram in the link below maps a PROM collection to action workflow that can be used to help review various electronic-based collection tools you are considering.
Step #5 – Interpretation of PRO Results
It is important to understand what domain the PROM is measuring and how it is scored in order to be able to utilize it appropriately, especially if it is to be shared with patients. Additionally, it is essential to be aware of how clinical significant change in scores between patients or within patients over time is defined and analyzed.
“Clinically significant change has been defined as changes in patient functioning that are meaningful for individuals who undergo psychosocial or medical interventions. Similarly, meaningful change is defined (from patient perspective) as one that results in a meaningful reduction in symptoms or improvement in function.” (Cella D. Hahn E.A.)
In PRO data reporting, minimally important differences (MIDs) represent a specific approach to measure clinical significance. They are defined as “the smallest difference in score in the outcome of interest that informed patients or informed proxies perceive as important. Although this statistical method may be necessary to utilize when reporting scores, it may vary by population and by context and some PROMs may already have known thresholds or meaningful cut points.
Therefore, the three main concepts to think about when interpreting PROM results are:
- Know the domain that is being measured and label it correctly
- Understanding the score and its meaning
- Understand the meaningful thresholds like MIDS and cut points (mild/moderate/severe impairment)
Further review of these statistical concepts may be necessary by those using a PRO program as they utilize PRO data.
Next Week: Wednesday, January 10, 2018 - Monitoring PRO Quality Measures: 5 Government Initiatives to Watch
Be sure to leave a comment in the form below!